Myopathy represents a heterogeneous group of muscle disorders characterized by abnormal structure or function of skeletal muscles. From genetic mutations to autoimmune processes, myopathies can stem from various etiologies, each presenting with unique clinical manifestations and prognostic implications. Accurate diagnosis and assessment of myopathy severity are paramount for guiding treatment decisions and prognosticating outcomes. Electromyography (EMG) and nerve conduction studies (NCS) emerge as indispensable tools in the diagnostic armamentarium, offering valuable insights into muscle function and pathology. This article explores the pivotal role of EMG/NCS in unraveling the complexities of myopathy, elucidating its diagnostic utility, and its significance in determining severity.
Understanding Myopathy: Myopathy encompasses a spectrum of disorders affecting skeletal muscles, characterized by weakness, fatigue, and impaired muscle function. Etiologies of myopathy are diverse, including genetic mutations, autoimmune processes, inflammatory conditions, metabolic disturbances, toxic exposures, and infectious agents. Clinical manifestations vary widely, ranging from proximal muscle weakness in genetic myopathies like Duchenne muscular dystrophy to symmetric muscle involvement in inflammatory myopathies such as polymyositis. Accurate diagnosis hinges on a thorough clinical evaluation, complemented by ancillary tests, including laboratory investigations, imaging studies, muscle biopsy, and neurophysiological assessments like EMG/NCS.
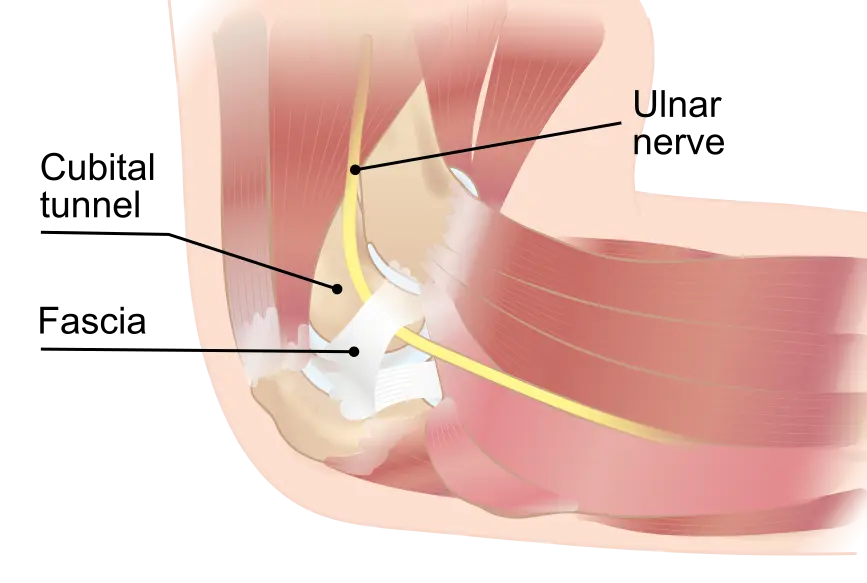
Role of EMG/NCS in Diagnosis: Electromyography (EMG) and nerve conduction studies (NCS) serve as cornerstones in the diagnostic workup of myopathy, offering invaluable insights into muscle function and pathology. EMG entails the evaluation of muscle electrical activity using needle electrodes, facilitating the identification of abnormal spontaneous activity, motor unit recruitment patterns, and assessing muscle fiber excitability. In myopathy, EMG may reveal characteristic findings such as fibrillation potentials, positive sharp waves, and myotonic discharges, indicative of muscle membrane instability and ongoing denervation processes.
Complementing EMG, nerve conduction studies (NCS) assess the integrity and function of peripheral nerves, aiding in the differentiation of primary muscle pathology from neuromuscular junction or nerve disorders. While NCS primarily evaluate nerve conduction velocity and amplitude, alterations in compound muscle action potentials (CMAP) and sensory nerve action potentials (SNAP) may provide indirect evidence of muscle pathology in myopathy. Additionally, the absence of conduction abnormalities may raise suspicion for primary muscle disease, prompting further evaluation with EMG and ancillary tests.
Diagnostic Challenges and Differential Diagnosis: Despite the diagnostic utility of EMG/NCS, distinguishing myopathy from other neuromuscular disorders can pose challenges, necessitating a comprehensive approach to differential diagnosis. Conditions mimicking myopathy include neuropathies, motor neuron diseases, neuromuscular junction disorders, metabolic myopathies, and musculoskeletal disorders. Hence, meticulous clinical correlation, coupled with judicious utilization of ancillary tests, remains paramount for accurate diagnosis and differentiation.
Assessing Severity and Prognosis: Beyond diagnosis, EMG/NCS play a pivotal role in assessing the severity and prognostication of myopathy, guiding therapeutic interventions and prognosticating outcomes. The extent of muscle involvement, characterized by the distribution and degree of weakness, aids in stratifying the severity of myopathy, ranging from localized muscle weakness to generalized, disabling impairment. Moreover, longitudinal monitoring of muscle electrical activity and nerve conduction parameters facilitates tracking disease progression, response to treatment, and prognostication of functional outcomes, thereby optimizing patient care and rehabilitation strategies.
Therapeutic Implications and Management: Armed with comprehensive diagnostic insights gleaned from EMG/NCS, tailored therapeutic interventions can be initiated to alleviate symptoms, mitigate disease progression, and optimize functional outcomes in myopathy. Management strategies encompass a multidisciplinary approach, incorporating pharmacotherapy, physical therapy, exercise regimens, and in select cases, immunomodulatory agents or surgical interventions. Additionally, addressing underlying etiologies, such as genetic counseling or metabolic optimization, holds paramount importance in halting disease progression and preventing complications.
Conclusion: Electromyography (EMG) and nerve conduction studies (NCS) stand as indispensable tools in the diagnosis, severity assessment, and therapeutic management of myopathy. By unraveling the intricacies of muscle function and pathology, EMG/NCS empower clinicians with invaluable diagnostic insights, guiding personalized treatment strategies, and optimizing patient outcomes. As we navigate the horizon of neurophysiological advancements, EMG/NCS continue to illuminate the path towards unraveling the complexities of myopathy, fostering innovation, and refining therapeutic paradigms to enhance the quality of life for affected individuals.