Introduction: Thoracic Outlet Syndrome (TOS) is a complex condition characterized by compression of the nerves and blood vessels passing through the thoracic outlet, located between the collarbone and first rib. It manifests with symptoms such as pain, numbness, tingling, and weakness in the upper extremities. Diagnosing TOS can be challenging due to its varied presentations and overlapping symptoms with other conditions. Electromyography (EMG) and Nerve Conduction Studies (NCS) play crucial roles in localizing the specific nerve involvement in TOS, aiding in accurate diagnosis and guiding appropriate treatment strategies.
Understanding Thoracic Outlet Syndrome: TOS encompasses a spectrum of neurovascular symptoms arising from compression of the brachial plexus, subclavian artery, or subclavian vein. This compression can occur due to various factors including anatomical anomalies, trauma, poor posture, repetitive overhead activities, or muscle hypertrophy. The condition is broadly classified into neurogenic, vascular, and non-specific types based on the structures primarily affected.
Clinical Presentation and Diagnostic Challenges: Patients with TOS often present with pain, weakness, and sensory disturbances in the neck, shoulder, arm, and hand. These symptoms can mimic those of cervical radiculopathy, carpal tunnel syndrome, or peripheral nerve entrapment, leading to diagnostic challenges. Furthermore, TOS can coexist with other musculoskeletal or neurological conditions, complicating the diagnostic process.
Role of EMG/NCS in Diagnosis: EMG and NCS are valuable diagnostic tools used to evaluate the function and integrity of peripheral nerves and muscles. In the context of TOS, these tests help localize the site of nerve compression and distinguish between neurogenic and non-neurogenic causes of symptoms.
- Electromyography (EMG): EMG involves the insertion of small needle electrodes into specific muscles to assess their electrical activity at rest and during voluntary contraction. In TOS, EMG findings may reveal denervation changes indicative of nerve injury or muscle dysfunction secondary to chronic compression. By analyzing the pattern and distribution of abnormal electrical activity, EMG can identify the specific nerves affected and differentiate between primary nerve injury and secondary muscle involvement.
- Nerve Conduction Studies (NCS): NCS measures the speed and amplitude of electrical signals transmitted along peripheral nerves. By applying surface electrodes to the skin and delivering controlled electrical impulses, NCS assesses nerve conduction velocity and amplitude, helping to identify areas of nerve dysfunction or demyelination. In TOS, NCS can detect abnormalities such as slowed conduction velocity or reduced compound muscle action potentials (CMAPs) indicative of nerve compression or injury within the thoracic outlet.
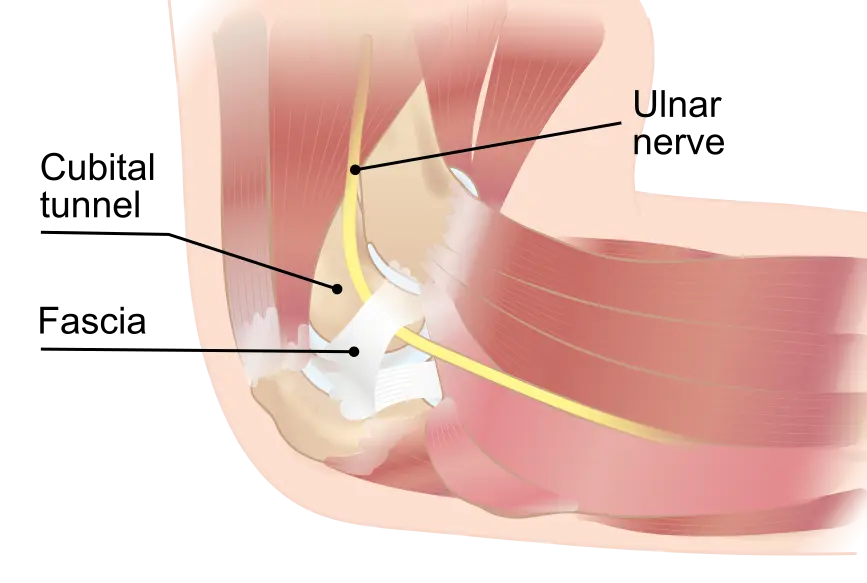
Localization of Nerve Involvement: EMG and NCS findings in TOS can provide valuable insights into the specific nerves affected and their anatomical distribution. Neurogenic TOS, the most common form, typically involves compression of the lower trunk of the brachial plexus or its branches, including the ulnar, median, and radial nerves. EMG/NCS studies may reveal abnormalities consistent with neuropathies affecting these nerves, such as decreased recruitment, abnormal motor unit potentials, or prolonged distal latencies.
In cases of vascular TOS, where compression of the subclavian artery or vein predominates, EMG/NCS may help rule out primary nerve involvement and identify secondary neurogenic changes resulting from ischemia or vascular compromise. However, it is essential to recognize that EMG/NCS findings alone may not be sufficient to diagnose vascular TOS, and additional imaging studies such as Doppler ultrasound or magnetic resonance angiography may be required to assess vascular abnormalities.
Challenges and Limitations: While EMG and NCS are valuable adjuncts in the diagnosis of TOS, certain limitations must be acknowledged. Variability in test interpretation, technical factors, and the presence of coexisting conditions can impact the accuracy of results. Additionally, false negatives can occur, particularly in cases of intermittent nerve compression or early-stage TOS where structural changes may be minimal. Therefore, clinical correlation and a comprehensive evaluation incorporating history, physical examination, and imaging studies are essential for accurate diagnosis and management.
Conclusion: Electromyography and Nerve Conduction Studies play pivotal roles in the diagnostic workup of Thoracic Outlet Syndrome, enabling clinicians to localize nerve involvement, differentiate between neurogenic and non-neurogenic causes, and guide appropriate treatment strategies. Despite their utility, these tests should be interpreted in conjunction with clinical findings and imaging studies to ensure accurate diagnosis and optimize patient outcomes in TOS management. Collaborative multidisciplinary approaches involving neurologists, physiatrists, vascular surgeons, and physical therapists are essential for comprehensive care and tailored treatment plans for individuals with Thoracic Outlet Syndrome.
Contact us today for more information.
Photo by: Karolina Grabowska