Electromyography (EMG) and Nerve Conduction Studies (NCS) are indispensable tools in neurology, offering valuable insights into the function and integrity of the peripheral nervous system. While Cubital Tunnel Syndrome (CTS) is often associated with ulnar nerve compression, EMG/NCS play a crucial role in diagnosing a spectrum of ulnar nerve conditions beyond cubital tunnel syndrome. This article explores the diverse applications of EMG/NCS in diagnosing various ulnar nerve disorders, shedding light on their significance in clinical practice.
Diagnosing Ulnar Nerve Conditions with EMG/NCS
The ulnar nerve, a major nerve of the upper extremity, innervates several muscles of the forearm and hand and provides sensation to the little finger and part of the ring finger. Dysfunction or compression of the ulnar nerve can lead to a range of symptoms, including pain, weakness, tingling, and numbness. EMG/NCS serve as powerful diagnostic tools in assessing ulnar nerve function, aiding in the diagnosis and characterization of various ulnar nerve disorders.
- Ulnar Nerve Compression at the Wrist (Guyon’s Canal Syndrome):
Guyon’s Canal Syndrome involves compression of the ulnar nerve as it passes through Guyon’s canal at the wrist. While primarily affecting the ulnar nerve, Guyon’s Canal Syndrome can lead to sensory disturbances in the ulnar nerve distribution and potentially affect adjacent median nerve function. EMG/NCS can help localize the site of ulnar nerve compression and differentiate between ulnar and median nerve involvement, ensuring an accurate diagnosis and guiding appropriate management strategies.
- Ulnar Nerve Compression in the Forearm:
Various anatomical anomalies or traumatic injuries can lead to ulnar nerve entrapment in the forearm, causing symptoms such as pain, weakness, and sensory deficits. EMG/NCS play a crucial role in localizing the site of ulnar nerve compression and assessing the severity of nerve dysfunction. By identifying specific patterns of nerve conduction abnormalities and muscle denervation, EMG/NCS facilitate targeted interventions, such as surgical release or conservative management, to alleviate symptoms and restore nerve function.
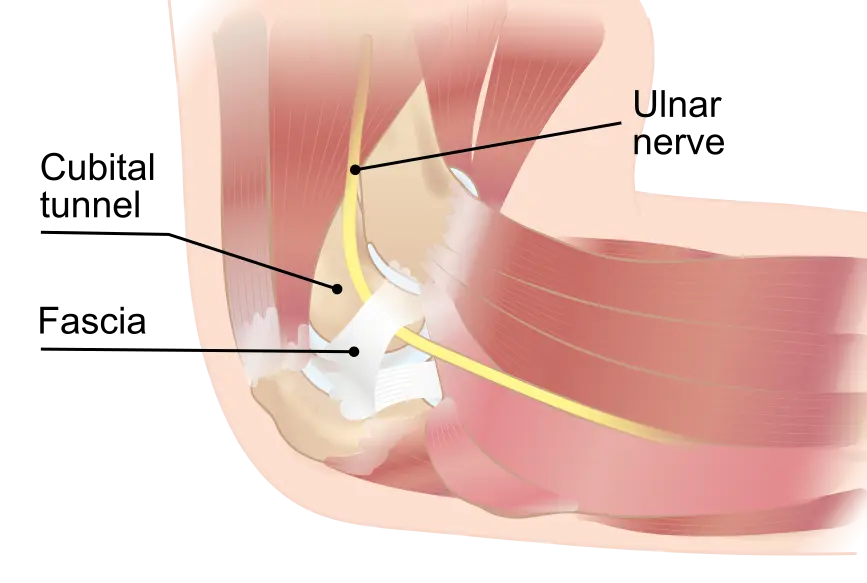
- Ulnar Nerve Compression at the Elbow (Cubital Tunnel Syndrome):
Although cubital tunnel syndrome is the most well-known ulnar nerve condition at the elbow, EMG/NCS can still provide valuable diagnostic information beyond confirming the diagnosis. These tests can assess the severity of nerve compression, differentiate between axonal loss and demyelination, and identify any associated muscle denervation. Additionally, EMG/NCS can help rule out other potential causes of ulnar nerve symptoms, ensuring a comprehensive evaluation and accurate diagnosis.
- Ulnar Nerve Compression at the Shoulder (Parsonage-Turner Syndrome):
Parsonage-Turner Syndrome, also known as brachial neuritis or neuralgic amyotrophy, is a rare condition characterized by sudden-onset severe shoulder pain followed by weakness and atrophy of the muscles innervated by the brachial plexus, including the ulnar nerve. EMG/NCS play a critical role in diagnosing Parsonage-Turner Syndrome by identifying denervation changes in the affected muscles and confirming the involvement of the ulnar nerve. These tests also help assess the extent of nerve damage and guide rehabilitation strategies to optimize recovery.
Conclusion
In conclusion, EMG/NCS are invaluable tools in diagnosing ulnar nerve conditions beyond cubital tunnel syndrome. By evaluating nerve conduction and muscle activity, these tests provide crucial diagnostic information, aiding in the accurate diagnosis and characterization of various ulnar nerve disorders. From Guyon’s Canal Syndrome to Parsonage-Turner Syndrome, EMG/NCS play a pivotal role in the comprehensive evaluation of ulnar nerve dysfunction, facilitating targeted interventions and improving patient outcomes in clinical practice.
Contact us today for more information.
Photo by: Edwintp