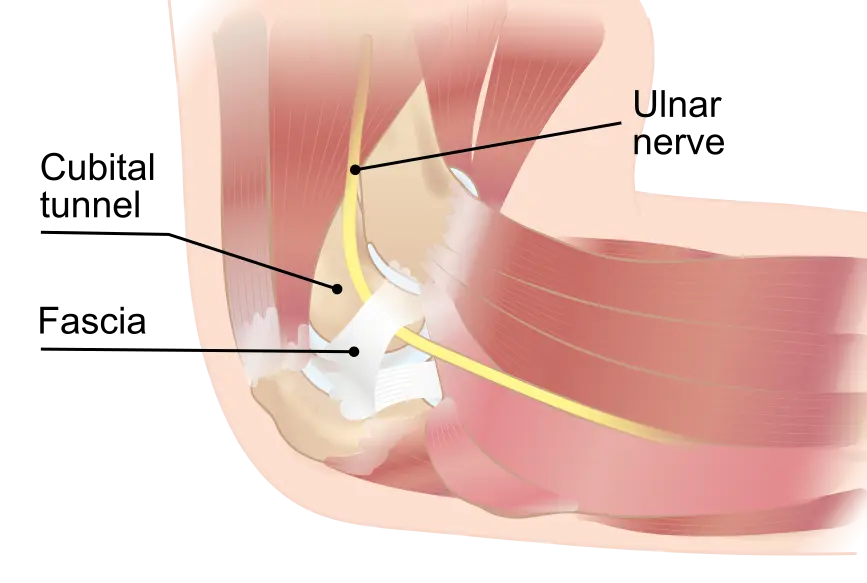
Cubital tunnel syndrome, also known as ulnar neuropathy at the elbow, is a common peripheral nerve entrapment disorder characterized by compression or irritation of the ulnar nerve as it passes through the cubital tunnel, located on the medial aspect of the elbow. This condition can lead to various symptoms, including numbness, tingling, weakness, and pain radiating to the forearm and hand, affecting daily activities and quality of life. Accurate diagnosis and assessment of the severity of cubital tunnel syndrome are essential for guiding treatment strategies and optimizing outcomes. In this article, we delve into the pivotal role of electromyography (EMG) and nerve conduction studies (NCS) in the diagnostic process, elucidating their utility in determining severity and aiding in therapeutic decision-making.
Understanding Cubital Tunnel Syndrome: Cubital tunnel syndrome arises from compression or irritation of the ulnar nerve, one of the major nerves supplying sensation and motor function to the forearm and hand. Etiological factors contributing to cubital tunnel syndrome include repetitive trauma, prolonged elbow flexion, anatomical variations, and systemic conditions such as diabetes mellitus or rheumatoid arthritis. Clinically, patients may present with symptoms such as numbness and tingling in the ring and little fingers, weakness in grip strength, and clumsiness in hand movements. Diagnosis is typically confirmed through a combination of clinical assessment, electrodiagnostic studies, and imaging modalities.
Role of EMG/NCS in Diagnosis: Electromyography (EMG) and nerve conduction studies (NCS) play a crucial role in the diagnosis of cubital tunnel syndrome, providing objective evidence of nerve dysfunction and localization of the site of compression. EMG involves the insertion of needle electrodes into specific muscles innervated by the ulnar nerve, such as the abductor digiti minimi or first dorsal interosseous, to assess for abnormalities in electrical activity. In cubital tunnel syndrome, EMG may reveal denervation changes, including fibrillation potentials and positive sharp waves, indicative of chronic nerve compression and muscle denervation.
Complementing EMG, nerve conduction studies (NCS) evaluate the integrity and function of peripheral nerves by measuring nerve conduction velocities and amplitudes. Specifically, for cubital tunnel syndrome, NCS assess sensory and motor conduction along the ulnar nerve pathway, typically at the elbow and wrist. Reduced conduction velocities and diminished sensory and motor nerve action potentials are indicative of nerve damage or dysfunction, further supporting the diagnosis of cubital tunnel syndrome and aiding in localization of the site of entrapment.
Diagnostic Challenges and Differential Diagnosis: While EMG/NCS provide valuable diagnostic information, differentiating cubital tunnel syndrome from other upper extremity neuropathies and musculoskeletal disorders can be challenging. Differential diagnoses may include other entrapment neuropathies (e.g., carpal tunnel syndrome), cervical radiculopathies, brachial plexopathies, or intrinsic hand pathologies. Therefore, a comprehensive clinical evaluation, including history, physical examination, and ancillary tests, is essential for accurate diagnosis and differentiation.
Assessing Severity and Prognosis: Beyond diagnosis, EMG/NCS play a crucial role in assessing the severity of cubital tunnel syndrome, guiding treatment decisions, and prognosticating outcomes. The extent of nerve dysfunction, characterized by the degree of sensory and motor involvement, aids in stratifying the severity of neuropathy. EMG/NCS findings, such as the amplitude of sensory and motor nerve action potentials, provide quantitative measures of nerve conduction and muscle function, which can be tracked over time to monitor disease progression and response to treatment.
Therapeutic Implications and Management: Armed with comprehensive diagnostic insights gleaned from EMG/NCS, tailored therapeutic interventions can be initiated to alleviate symptoms, mitigate nerve compression, and optimize functional outcomes in cubital tunnel syndrome. Management strategies may include conservative measures such as activity modification, splinting, and physical therapy to alleviate symptoms and prevent further nerve damage. In refractory cases or those with significant nerve compression, surgical interventions such as ulnar nerve decompression or transposition may be considered to alleviate symptoms and prevent complications such as muscle wasting or irreversible nerve damage.
Conclusion: Electromyography (EMG) and nerve conduction studies (NCS) serve as indispensable tools in the diagnosis, severity assessment, and management of cubital tunnel syndrome. By providing valuable insights into nerve function and pathology, these neurophysiological tests aid in confirming the diagnosis, localizing nerve injury, and guiding treatment decisions. As our understanding of cubital tunnel syndrome continues to evolve and new technologies emerge, EMG/NCS will remain essential components of the diagnostic and therapeutic armamentarium, helping to optimize outcomes and improve the quality of life for affected individuals.